Arrhythmias¶
Acute management¶
- 12-lead EKG if possible and have defib pads on patient
- Is the pt unstable (hypotensive, signs/symptoms of hypoperfusion)?
- Is the information real?
- Review tele strips if stable: VUMC Web Resources -> VUH PIICiX Philips Web -> patient selection -> alarm review (vuhphilipsweb.app.vumc.org)
- Review past EKGs to determine if patient has had this rhythm before
- Ensure pt has good IV access
- Labs: BMP, Mg, TSH, and ± troponin, tox screen
Bradyarrhythmias - Lin Cao¶
Background¶
- Broadly classified as sinus node dysfunction (pacing defect) or atrioventricular block (conduction defect)
- Clinical presentation varies widely based on underlying cause,
timing, degree of block/dysfunction
- Unlikely to cause symptoms if HR >50
- Symptoms include syncope/presyncope, dyspnea, angina
Potential Etiologies¶
- Infection (including perivalvular abscess from endocarditis)/sepsis
- Ischemia
- Rheumatologic/Inflammatory
- Post-cardiac surgery
- Hypothyroidism
- Sleep apnea
- Infiltration (amyloid, hemochromatosis)
- High vagal tone (pain, nausea)
- Medications: Antihypertensives, antiarrhythmics, psychoactive meds, anesthetics, cannabis, muscle relaxants, etc.
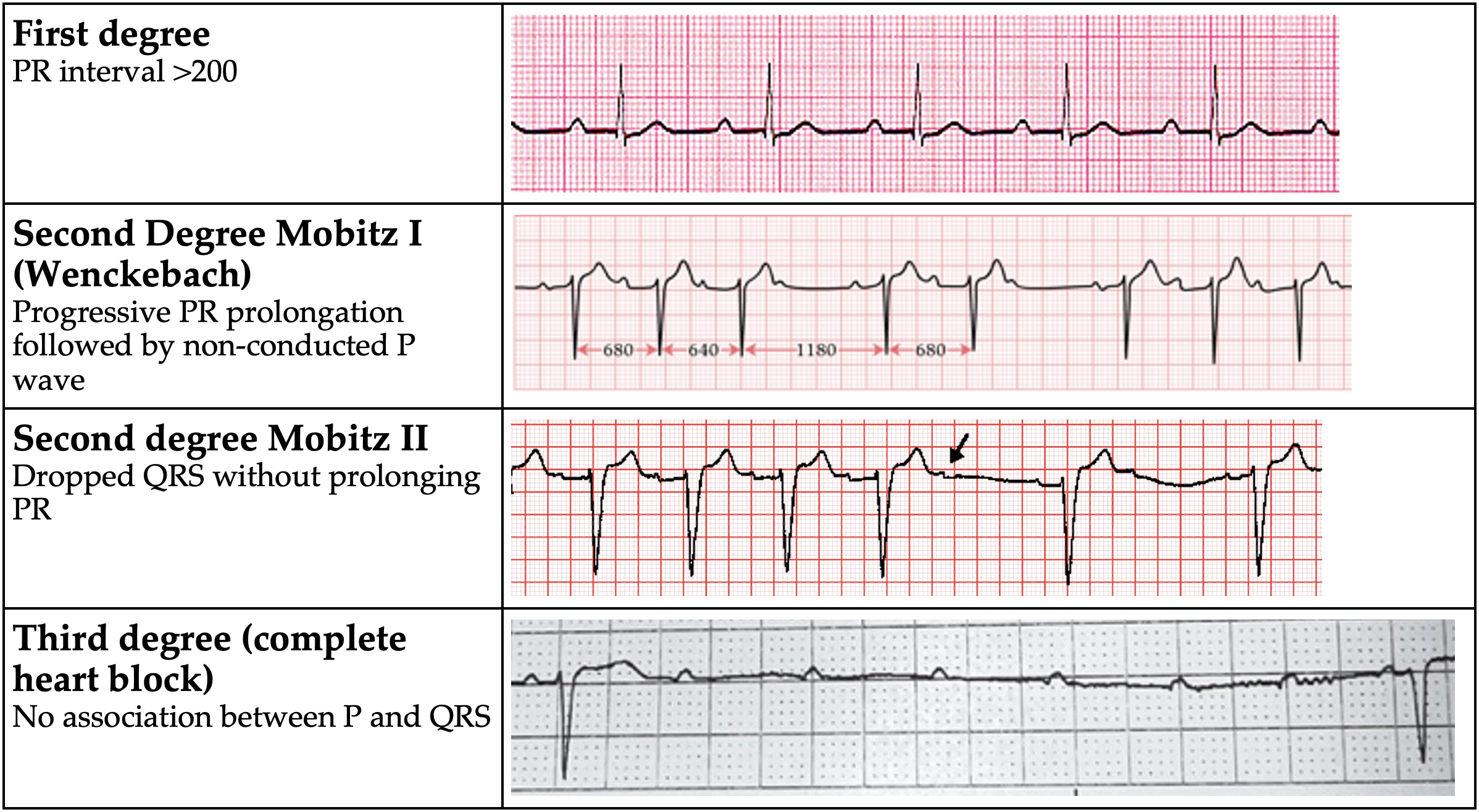
AV Block
Evaluation¶
- TTE if structural disease suspected
- Ambulatory cardiac monitoring if frequently symptomatic
Management¶
- Avoid nodal blocking agents – Adenosine, Beta-blockers, CCBs, Digoxin
- Observation if asymptomatic
- Treat identified underlying causes
- If symptomatic or high-grade block (Mobitz II or complete heart block), EP consult for pacemaker evaluation
- If unstable:
- Atropine (0.5 mg every 3 to 5 minutes; maximum total dose: 3 mg)
- Do NOT use in heart transplant
- Call CCU Fellow
- Dopamine (5 to 20 mcg/kg/minute) OR Epi (2 to 10 mcg/min)
- Transvenous pacing (Pacer pads on the defib device are capable of pacing, but don’t forget to sedate!)
Tachyarrhythmias - Narrow complex - Manasa Atyam¶
Background¶
- Three causes of tachyarrhythmias
- Re-entry: patient with structural heart disease (ex post-infarction scar)
- Abnormal Automaticity: electrolyte abnormalities or acute ischemia (Purkinje fibers)
- Triggered Activity: early and late after depolarizations. Ex: Hypokalemia, ischemia, infracts, excess calcium and drug toxicity
Evaluation¶
- Unstable tachyarrhythmia
- Start with treatment, determine type later
- Synchronized cardioversion: place defibrillator pads, consider 0.5-2mg IV midazolam for sedation, prepare for synchronized cardioversion at 200J (can ↑ to 300-360 J)
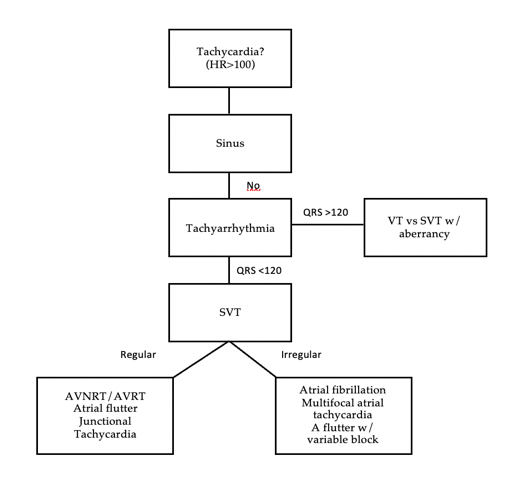
Tachyarrhythmia differential
Management¶
- Sinus tachycardia- Almost always secondary
- Address underlying causes: fever/sepsis, hypo/hypervolemia, anxiety, anemia, PE, ACS, hypoxia, pain, urinary retention, withdrawal
- Atrial Fibrillation/Flutter – See Atrial fibrillation section
- AVNRT/Orthodromic AVRT
- Look for p buried in QRS, rate 150-250, AVRT will have delta waves when NSR
- Vagal maneuvers (1st line): Sit patient upright have them blow into tip of 10cc syringe for 10-15 seconds rapidly lay supine and raise legs
- Adenosine (2nd line): therapeutic (break AVRT/AVNRT) and diagnostic
(allows visualization of underlying rhythm)
- Do NOT give in heart transplant, severe COPD, pre-excitation causing wide complex tachycardia (WPW antidromic AVRT)
- Peripheral line at AC or above w/ arm elevated: 6mg x1, 6mg x1 (if not effective after 1-2 min), 12mg x1 (if refractory to 6mg)
- Central line: cut dose in half to 3mg x1, 3mg x1, 6mg x1
- Multifocal atrial tachycardia
- 3 or more p wave morphologies. Seen in cardiac and pulmonary disease
- Usually does not cause hemodynamic instability
- BBs and non-DHP CCBs can be effective, need to address underlying issue
| Drug | Dosing | Benefits | Side Effects |
|---|---|---|---|
| Metoprolol | 5mg IV q5m x3 PO metoprolol tartrate 12.5mg q6 hours ↑ every 6 hr to target |
Good 1st line agent Less BP effect than dilt |
Hypotension, Negative inotropy |
| Diltiazem | 10-20 mg IV over 2m q15m x2 drip = 5-15 mg/hr |
Good 1st line w/ normal EF with drip needed | Hypotension Avoid in HFrEF |
| Esmolol | 500 mcg/kg bolus drip = 50-200 mcg/kg/min |
Rapid onset/offset RBC metabolism |
Hypotension |
| Amiodarone | 150 IV over 10-30m, then 1 mg/m for 6h, then 0.5mg/m for 18h | Minimal BP effects Long lasting; Relatively fast onset (acute effect is mostly beta blockade) |
Pulmonary and thyroid toxicity Cardioversion |
| Digoxin | 500mcg IV x1, then 250mcg IV q6h x2-3 | Great for reduced EF, positive inotropy | Slow onset Depends on vagal tone – poor in hyper- adrenergic states |
| Procainamide | 20-50 mg/min loading, 1-4 mg/min maintenance | Use in pre-excitation syndromes (i.e. WPW), does not inhibit AV nodal conduction | Lupus-like syndrome Hypotension |
Tachyarrhythmias - Wide Complex and PVCs¶
Manasa Atyam
Definitions¶
Ventricular tachycardia (VT): a run of 3+ PVCs
- Sustained VT: VT for 30 seconds or shorter if it requires intervention
- Nonsustained VT (NSVT): VT for \< 30 seconds
- VT storm: 3+ separate episodes of sustained VT within 24 hrs.
VT Morphologies
- Monomorphic VT: similar QRS configuration from beat to beat
- Usually 2/2 scar-mediated VT from prior infarction
- Polymorphic VT: a continuously changing QRS configuration from beat
to beat
- Ischemia until proven otherwise
- Torsades de Pointes (TdP): a form of polymorphic VT with a continually varying QRS that appears to spiral around the baseline of the ECG in a sinusoidal pattern
- Ventricular fibrillation (VF): chaotic rhythm characterized by undulations that are irregular in timing and morphology, without discrete QRS complexes
Ventricular Tachycardia vs. SVT with aberrancy
- VT: The action potential originated in the ventricles (ex: VT)
- Supraventricular tachycardia with aberrancy: the action potential originates from a focus above the ventricles & conducts through the AV node with a delay or block resulting in a wide QRS (mimics VT)
- Ex: sinus tachycardia w/ bundle branch block (block may be rate dependent), AF w/ LBBB
Many ways to differentiate VT vs. SVT w/ aberrancy
- Consult cardiology for assistance
- Look for ECG features suggestive of VT
- Very broad complexes >160 ms
- RsR’ complex with a taller left rabbit ear In V½
- AV dissociation (P/QRS dissociation)
- Capture Beats: native QRS complexes making a cameo during the VT
- Fusion Beats: QRS which appears like a signal average of VT and native complex
- There are more advanced criteria to help distinguish. The aVR (Vereckie) criteria is one example that is fast and accurate
Management¶
Unstable
- Sedate with midazolam 1-2mg
- Cardioversion for monomorphic VT. Synchronized shock at 100-200J
- Defibrillation if VF/polyVT
Stable
- Medications (as below)
| Drug Name | Dosing | Mechanism | Side Effects |
|---|---|---|---|
| Amiodarone | 150mg IV over 10 min, then 1mg/min for 6 hours; repeat bolus if VT recurs | Class III -K+ channel blocker; has class Ia, II, & IV effects |
Bradycardia, hypotension (acutely) |
| Lidocaine | 1-1.5 mg/kg (usually 75-100 mg) at a rate of 25-50mg/min; lower doses of .5-.75mg/kg can be repeated every 5-10 min as needed | Class IB -fast Na+ channel blocker-> slows conduction |
Slurred speech, AMS, seizures, bradycardia |
| Procainamide | 20-50mg/min until arrhythmia terminates or max dose 17mg/kg is reached | Class IA -fast Na+ channel blocker -> slows conduction -K+ channel blocker-> prolongs repolarization |
Bradycardia, hypotension, torsades, drug-induced lupus Avoid in HF pts, prolonged QT |
-
Cardioversion If refractory to medical management
-
Treatment of underlying cause if identifiable
- Ischemia, electrolyte disturbances, heart failure, drugs
Premature Ventricular Complexes (PVCs)¶
Background¶
- Premature Ventricular Complex (PVC): early ventricular depolarization ± mechanical contraction
- PVC burden: % of beats of ventricular origin / total beats over a 24h period
- PVCs are common: Up to 80% of apparently healthy people have PVCs
- Normal number of PVCs in an adult is \<500 in 24h
Etiologies¶
- HTN with LVH, prior MI/scar, HF, myocarditis, ARVC, HCM, idiopathic VT, OSA, pHTN, COPD, thyroid disease, substance use (EtOH, nicotine, stimulants, caffeine)
Inpatient Evaluation & Management¶
- 12 lead EKG: conduction disease, long QT syndrome, Brugada syndrome, ARVC
- Labs: K, Mg, TSH, drug screen
- Evaluate for QT prolonging agents (risk of Torsades)
- Evaluate tele for PVC burden
- Inpt consult to EP for PVCs rarely warranted unless significant PVC burden (>5 PVC/min, consistently) in setting of reduced LVEF.
- For pts with >5 PVC/min or pts with symptoms, discharge with Ziopatch (VA) or mobile cardiac telemetry (VU) and obtain TTE if none recent.