Brown Recluse Bites (Loxoscelism)¶
Ashley Zeoli
Background¶
- Only a handful of spiders are truly harmful to humans
- The brown recluse (a member of the Loxoceles genus) is widespread in the South, West, and Midwest US
- They are often found in homes (attics, basements, cupboards) and outdoors (rock piles and under tree bark)
- Their numbers increase in association with humans (i.e. synanthropic)
- Appearance/identification:
- Brown recluses have three pairs of eyes, a monochromatic abdomen and legs, and very fine hairs on its legs
- Using the “violin” pattern on its body is a poor way to identify this spider, as other harmless spiders can have similar markings.
- Loxocelism is the medical manifestation of the brown recluse spider bite
- Venom contains insecticidal toxins, metalloproteases, and phospholipases
Presentation¶
- Bites are most common on the upper arm, thorax, or inner thigh
- Local signs:
- Sometimes painless, but can cause burning sensation with two small cutaneous puncture marks with surrounding erythema. Pain can increase over the first 8 hours
- Usually appears as a red plaque or papule with central pallor and can sometimes present with vesiculation
- Usually self-resolves in 1 week
- Skin necrosis:
- In some, skin lesion can progress to necrosis overall several days
- An eschar will form that eventually ulcerates
- Usually will heal over several weeks to months
- Systemic signs:
- The degree of systemic effects does not correlate with the appearance of the bite
- Symptoms may develop over several days, and include nausea, vomiting, fever, rhabdomyolysis, malaise, acute hemolytic anemia, significant swelling from head/neck bites that can compromise the airway, DIC and renal failure
Evaluation¶
- Presumptive diagnosis is based clinical presentation of the bite/wound
- DDx includes vasculitis, pyoderma gangrenosum, cellulitis, or other arthropod bites
- Definitive diagnosis is based upon observing a spider bite in combination identification by an entomologist. There is an assay for Loxoceles venom, but it is not commercially available
- Patients with local symptoms do not need any further workup
- Patient with any systemic symptoms require lab evaluation for more
serious disease:
- CBC, UA to eval for blood, CMP, CK
- If anemia: Type and Screen, peripheral smear, reticulocyte count, LDH, haptoglobin, coags to evaluate for hemolysis or DIC
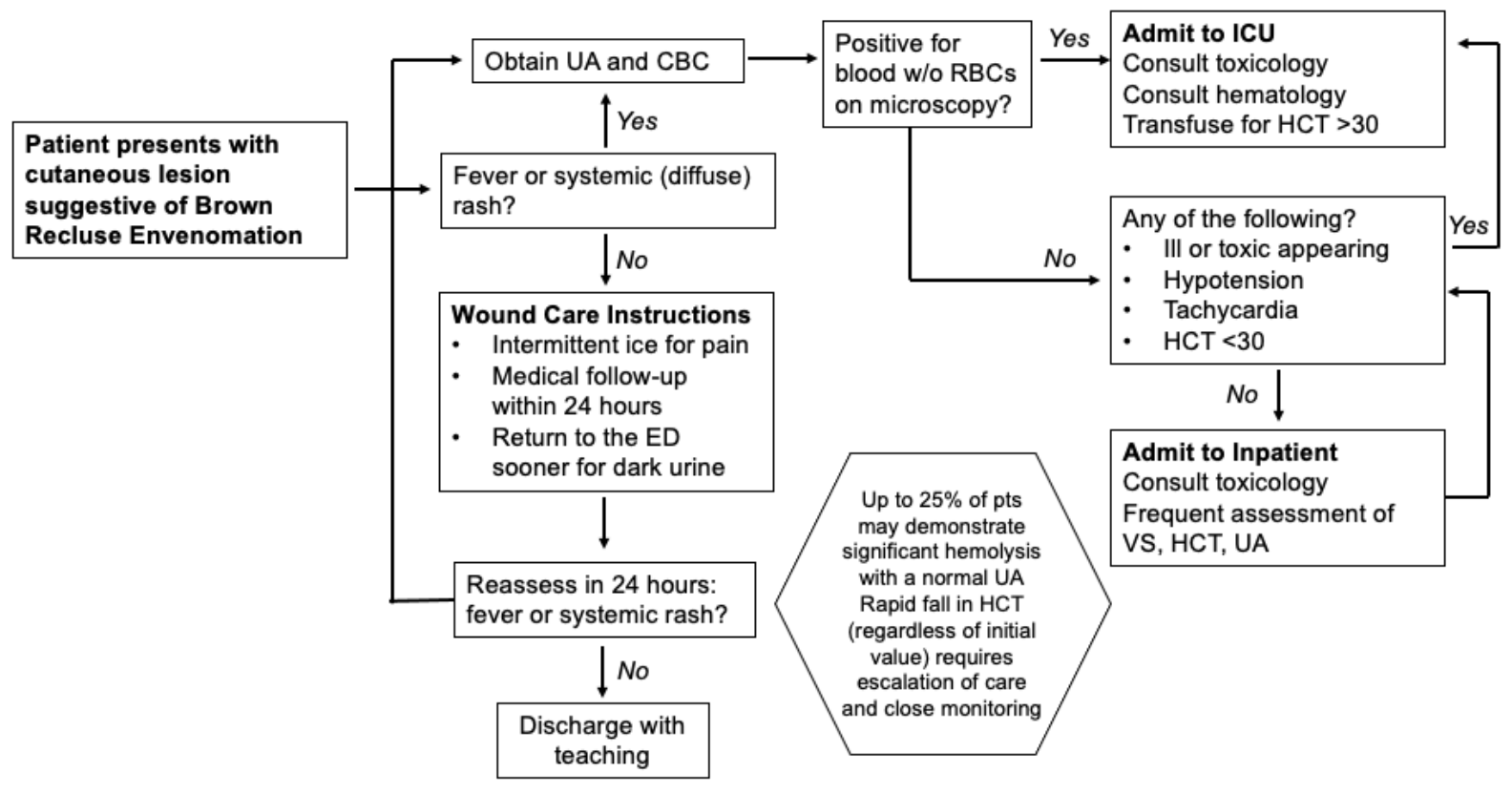
Loxocelism flowchart
Management¶
- Local signs:
- Wound care (soap/water, elevation)
- Pain management
- Tetanus vaccine/prophylaxis if indicated
- Antibiotics only if signs of concurrent cellulitis
- Skin necrosis:
- Symptomatic and supportive care
- Surgical intervention can worsen cosmetic outcomes and is rarely indicated in the acute care setting. Skin grafting is occasionally needed for a very large ulcerative wound that is not healing. Infection is rare, Furthermore, the ulcerative base of the wounds often have a yellow stringy material that is not pus or infection. Please call Toxicology with any questions regarding brown recluse bites
- Systemic signs: Targeted at treatment of symptoms that develop (Consult toxicology)
- Hemolytic anemia: transfuse for Hgb <10 + consult heme
- Rhabdomyolysis: LR for UOP >200-300cc/hr
- If patient develops chest pain, obtain EKG and check a troponin; if either is abnormal please obtain echo and call Toxicology as heart effects (i.e. myocarditis) is something we have been seeing at VUMC
- DIC: supportive care