Bedside Echocardiography¶
Jamie Pfaff
Finding an Ultrasound¶
- MICU: radiology room behind charge nurse's desk in middle hallway
- VA ICU: In front of resident workspace
- 8N: Behind nursing station before entering cleaning supply room
- 8S: In supply closet to left as you walk toward nursing station - (door code is 1-3-5)
- 6MCE: COVID restricted (ask nurses)
- CCU/5N only: supply room on left as entering CCU
- Round wing: 5th floor, ask nurses
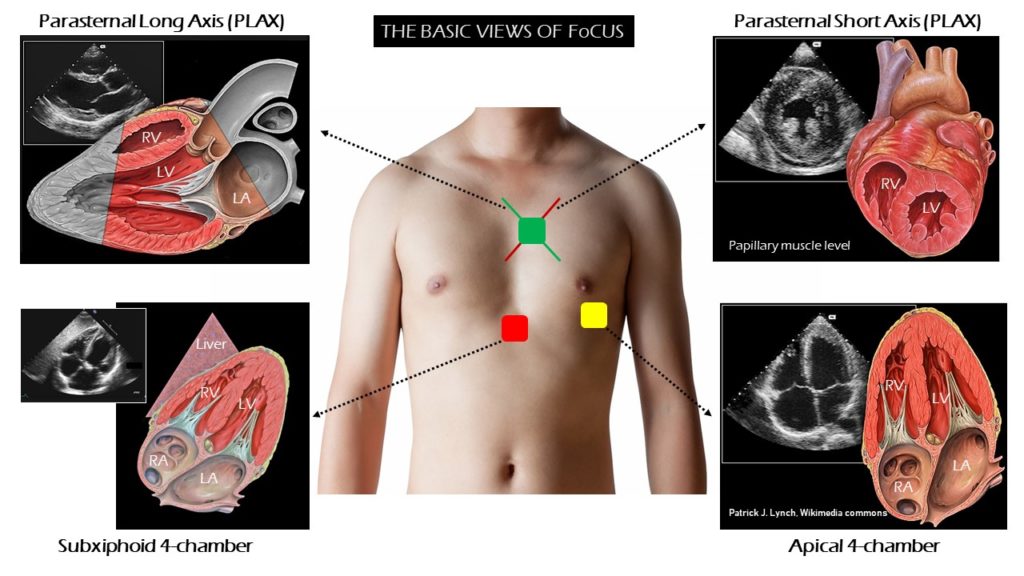
TTE Standard Views¶
Parasternal long¶
- Probe position: Rotate probe 180 degrees with right edge of probe/probe marker pointing toward pt’s left shoulder
- Make sure probe is centered over mitral valve (In right spot if you can see MV and AV)
- E Point Septal Separation (EPSS)
- Distance separating the anterior MV leaflet from the septal wall as measure of LV systolic function (easy evaluation of systolic function)
- Place M mode spike at tip of mitral leaflet and hit M mode (perpendicular to septum)
- Identify E point (passive filling of LV) and determine distance
from interventricular septum (IVS)
- <7mm = Normal
- >10mm = HF
- Confounders that elevate EPSS: AR, MS
Parasternal short¶
- Probe position: Rotate probe 180 degrees with right edge of probe/probe marker pointing toward patient’s left shoulder
- Good position to assess EF by visualizing wall thickening
Apical four chamber¶
- Probe position: Slide down and look near patient’s left nipple (or in the intermammary fold after lifting up breast tissue if needed - at PMI if able to palpate)
- Good to assess EF by visualizing cardiac shortening
Subxiphoid¶
- Probe position: Push probe head into pt’s abdomen just below xiphoid and flatten probe to make nearly parallel to pt’s position, marker to pt’s left
- Troubleshooting: shift probe slightly left of midline (toward pt’s right) and angle toward heart/right to use liver as acoustic window or ask pt to take big breath (moves heart closer to probe)
- Best window to visualize pericardial effusion
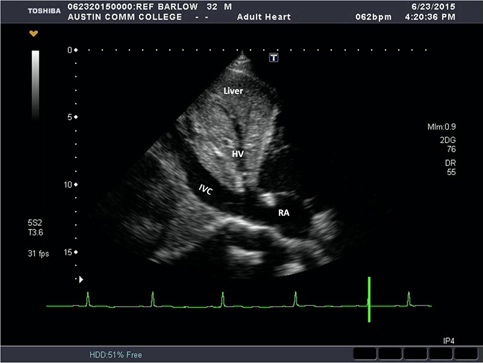
IVC¶
- Probe position: subxiphoid area with probe marker facing toward pt’s head tilted slightly left of midline, trace IVC into RA to verify correct vessel (vs aorta)
- IVC size and collapsibility used as a surrogate for CVP and RAP
- <2.1 cm and >50% collapse: RAP ~3mmHg
- <2.1 cm and < 50% collapse or >2.1cm and >50% collapse: RAP ~8mmHg
- >2.1cm, <50% collapse: RAP ~ >15mmHg
Resources¶
- https://www.coreultrasound.com/basic-cardiac-function/
- http://pie.med.utoronto.ca/tte
- https://www.echocardiographer.org/TTE.html
- App: FATE CARD (Focus Assessed Transthoracic Echocardiography) https://test.usabcd.org/fate-card/ https://apps.apple.com/us/app/fate-card/id413628612