Right Heart Catheterization¶
Ahmad Yanis
Pulmonary artery catheter (PAC): Multilumen catheter that sits in the right heart to provide invasive measurement of hemodynamic parameters
Indications for PAC placement¶
-
Diagnose undifferentiated shock
-
Severe cardiogenic shock
-
Diagnose pulmonary hypertension
-
Diagnose left -> right shunting
-
Diagnose valvular and pericardial disease
-
Titrating medications, specifically inotropes, pulmonary vasodilators, diuresis
Contraindications to PAC placement¶
-
Infection at the insertion site
-
RA/RV mass or thrombi
-
Tricuspid or pulmonic valve endocarditis
-
Mechanical tricuspid or pulmonic valves
-
Presence of RV assist device
Complications of PAC placement¶
-
Arrythmias: VT, RBBB, 3rd degree AV block if preexisting LBBB
-
Infection (endocarditis of the pulmonary valve)
-
Bleeding
-
Pulmonary embolism and pulmonary Infarct
-
Pneumothorax
-
Air embolism
-
Pulmonary artery perforation / rupture
-
Endocardial/valvular damage
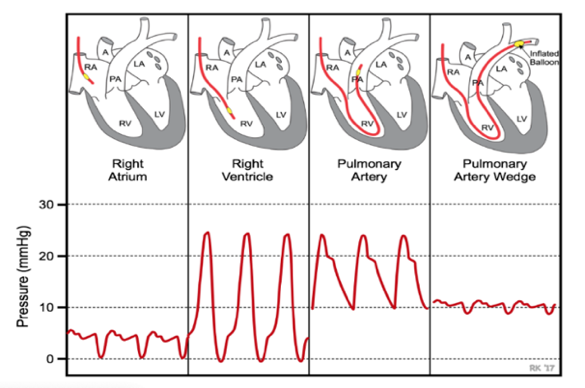
PAC Pressure Tracings¶
| Definition | Normal "Rule of 5s" |
|
|
|---|---|---|---|
Central Venous Pressure (CVP) |
Pressure in superior vena cava, often an indicator of volume status | 0 - 5 mmHg | Elevated CVP is indicative of cardiac dysfunction and/or fluid
retention Low CVP is indicative of volume depletion or decreased venous tone |
| Right Atrial Pressure (RAP) | Surrogate for preload, should be same as CVP | 0 - 5 mmHg | Elevated with disruption in forward cardiac flow or increase in intravascular volume |
| Right Ventricle Pressure ( | Right ventricular systolic and diastolic pressures; RVSP can be surrogate for PASP | 25/5 mmHg | Elevated with diseases that elevate PA pressure and pulmonic valve disorders. Severe RVP elevations are generally chronic while acute conditions typically have RVSP <40-50. |
| Pulmonary Artery Pressure (PAP) | Measured as systolic, diastolic, and mean pressures. Diagnoses pHTN. | 25/10 mmHg Mean: 10 - 19 mmHg |
Elevated In acute conditions (PE, hypoxemia induced pulmonary vasoconstriction) or pHTN (mean PAP > 20 mm Hg) |
| Pulmonary Artery Wedge Pressure (PAWP or wedge) | Pressure measured by wedging the PAC into a small pulmonary arterial branch; surrogate for left atrial pressures and LVEDP | 10 mm Hg | Increased with elevated LVEDP: systolic or diastolic heart failure, mitral and aortic valve disorders, hypervolemia, R to L shunts, tamponade, constrictive/restrictive cardiomyopathy |
| Thermodilution Cardiac Output & Index | Amount of blood pumped in one min. CI is the cardiac output divided by body surface area (to standardize for body size) | CO: 3.4-15 L/min CI: 2.8-4.2 L/min/m^2 |
Low CI: systolic/diastolic heart failure, severe valvular disorder (MR, AS), RV failure, pHTN, cardiogenic shock. Elevated CI (high-output state): sepsis, anemia, thyrotoxicosis, A-V shunt |
Mixed central venous oxyhemoglobin saturation (SvO2) |
% of oxygen bound to Hgb in blood returning to the right side of the heart, reflects total body O2 extraction | 65-70% | High SvO2 (> 65%) = decreased O2 demand or “high flow” states seen in distributive shock (sepsis) Low SvO2 (< 50%) = decreased O2 delivery seen in cardiogenic or hypovolemic shock. In low SvO2 states, there is less O2 supply to same demand) |
Calculating Hemodynamic Parameters from PAC Pressures¶
| Definition | Normal Values | Interpretation | |
|---|---|---|---|
| Fick CO and CI | Calculated CO based on Oxygen consumption (VO2), Hbg, and O2 sats of arterial and venous blood | 4-7 L/min 2.5-4 L/min/m2 |
See "Cardiac Index" above. |
| Systemic Vascular Resistance (SVR) | Measurement of afterload; helpful in delineating the etiology of shock as well as guiding afterload-reduction therapy in HFrEF | 700-1200 dynes*s*cm-5 | Elevated SVR is seen in hypovolemic, cardiogenic, and obstructive shock Decreased SVR is seen in distributive shock (sepsis, anaphylaxis, neurogenic) |
| Transpulmonary gradient (TPG) | Differentiates between pre- and post-capillary pulmonary hypertension. | < 12 mmHg | A TPG value greater than 12 mmHg indicates that a component of the pHTN is secondary to pulmonary vascular disease |
| Pulmonary Vascular Resistance (PVR) | Gold standard in the estimation of the severity of pre-capillary
pHTN Reflects the pressure drop across the pulmonary system only and is independent of the LA, mitral valve and the LV |
< 3 Wood Units 30-90 dynes*sec*cm5 |
Elevated PVR (>3 Wood units) suggests pre-capillary pHTN Normal PVR seen in pulmonary venous hypertension (diastolic dysfunction) |
| Pulmonary artery pulsatility index (PAPi) | Pulmonary pulse pressure relative to preload (RAP), Indicator of RV function | > 0.9 | PAPi < 0.9 predicts in-hospital mortality and/or need for RVAD in acute MI. Can be decreased in pure RV failure or biventricular failure |
| Cardiac Power | Cardiac output relative to afterload, a measure of LV contractile reserve | Normal > 1 | CP< 0.6 strongly suggestive of LV failure Found to be a strong independent hemodynamic correlate in pts with cardiogenic shock. Predictor of mortality in CCU |