ICU Delirium¶
Phil Schmitt
Background¶
- Delirium is a DSM-V diagnosis based on acute-onset fluctuating attention and awareness, unlike the chronic changes seen in dementia. It is largely interchangeable with Encephalopathy.
- This becomes more difficult to assess when patients are sedated, intubated, etc. in the ICU
- Very well-studied at VUMC, more resources found at: https://www.icudelirium.org.
- Associated with higher morbidity and mortality compared to those who do not experience delirium and duration of delirium also associated with higher morbidity and mortality.
Evaluation¶
- Can present as either hyperactive (agitated, trying to leave bed, etc.) or hypoactive (somnolent, minimally interactive, etc.).
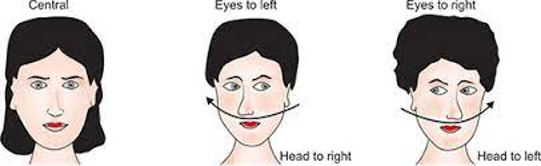
- Do neuro exam to rule out focal deficits. Basic ICU/coma neuro exam detailed below:
- For ICU Patients, consider sedation when doing neuro exam - propofol and other anesthesia dampens brainstem + peripheral reflexes
- Always remember patients can be encephalopathic and evolve another acute neurological syndrome. Follow up any odd/changing exam findings.
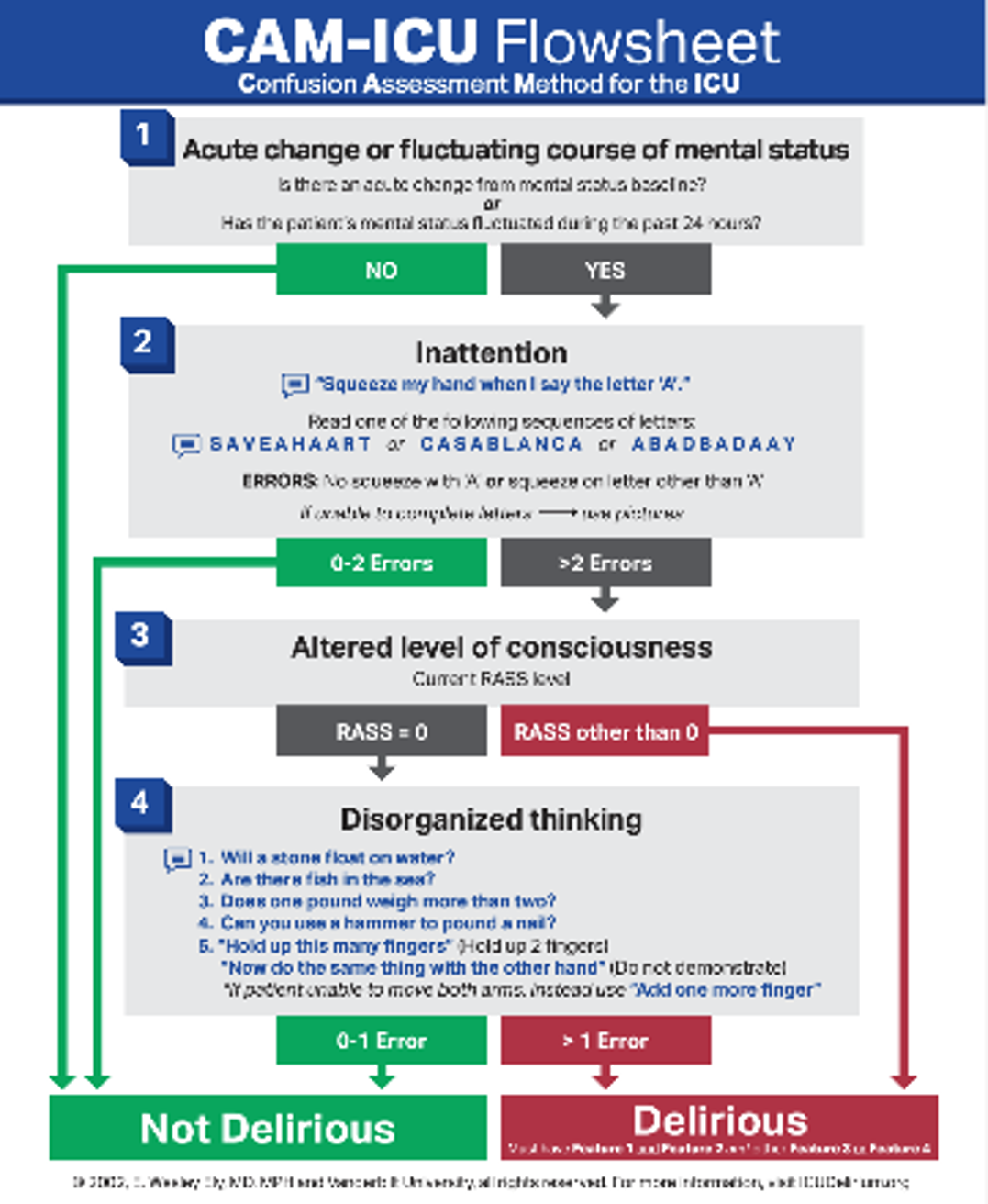
- Perform the CAM-ICU for scoring – ICU nurses perform this q4h as part of routine ICU care
- See RASS scoring table in ABCDEF Bundle Critical Care chapter.
Differential Diagnosis¶
- Most typically due to changes in environment, alterations in sleep cycle, reduced cognitive reserve from critical illness, dementia, neurodegeneration, etc.
- other differentials fit in a modified VITAMINS PO mnemonic
| Category | Causes |
|---|---|
| Vascular | Ischemic stroke, CNS hemorrhage, arrhythmia, carotid stenosis |
| Infectious |
|
| Trauma | Falls, TBI, etc. |
| Autoimmune | Autoimmune encephalitis, SLE, CNS vasculitis among others |
| Metabolic |
|
| Ingestion |
|
| Neoplasm | Brain mets, primary CNS tumors, CA associated with paraneoplastic syndromes (SCLC, Multiple myeloma, ovarian teratoma, etc.) |
| Seizure | |
| Pain | Always important to consider, especially in geriatric pts |
| Oxygenation | Hypoxia |
Management¶
- Initial toxic/metabolic/infectious workup can include: CBC, CMP, TSH, Folate, Vitamin B12, UA, blood cultures, CT Head w/o. Look through med list to see if there are any sedating medications that could be contributing and try to minimize as much as possible.
- Definitive treatment is addressing underlying etiology.
- First-line symptomatic treatment includes delirium precautions, such as keeping blinds open during daytime, limiting daytime naps, redirection when agitated, lights on during day, TV on during day, family at bedside (opposite of these at night). There is an order in Epic called Nursing: Delirium Care, which can be found as part of the Geriatric Delirium Care order set, that has all these precautions listed out.
- Although they do not provide mortality benefit in ICU delirium patients (and debatably worsen mortality), antipsychotics can be used if needed for more severe agitation IE pulling at lines, physical aggression. Start with one-time dose of zyprexa 2.5 mg or 5 mg, can escalate to 1 mg haldol if refractory. Check an EKG for QTc prolongation (>440ms) prior to giving.