Opioids: General Principles & Conversion¶
Eli Cohen
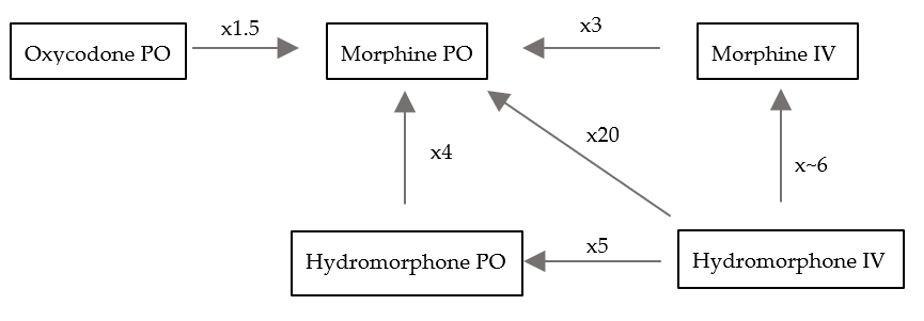
Oral Morphine Equivalent (OME) Conversion Table:¶
| Drug | PO | IV | APAP | IR | ER | Notes |
|---|---|---|---|---|---|---|
| Tramadol | 0.1x | - | - | Tramadol | Ultram ER™ | NSAID properties |
| Morphine | 1x | 3x | - | Morphine IR | MS-Contin™ | Renally cleared |
| Hydrocodone | 1x | - | Lortab | Hydrocodone | NA | |
| Oxycodone | 1.5x | - | Percocet | Roxicodone™ | Oxycontin™ | |
| Hydromorphone | 4x | 20x | - | IV, Oral | - | Oral is $ |
| Fentanyl | 300x | 300x | - | IV, Buccal, Nasal | Patch | Dosed in ug, not mg |
- Abbreviations: ER, extended release; IR, immediate release; IV, intravenous; PO, oral; APAP, Acetaminophen
Pharmacokinetics:¶
| Mechanism | Onset | Peak Effect | Duration |
|---|---|---|---|
| PO | 30 min | 1 hr | 3 – 4 hrs |
| IV | 5 min | 15 min | 1 – 2 hrs |
Conversion:¶
- Transition between opiates is done using oral morphine equivalents (OMEs). Each drugs’ potency is compared to oral morphine (see table). Ex: 1 mg IV morphine = 3 mg PO morphine
- When titrating doses, you can increase the dose by 25-50% for moderate pain and 50-100% for severe pain
- When transitioning, doses are traditionally reduced by ¼ to ⅓ due to cross tolerance; however, if the pain is uncontrolled, it is reasonable to not dose reduce to account for this.
- IR/ER regimens: Consider switching to extended release when requiring 3-4 doses of intermediate release (IR) medications in a 24-hour period regularly. The ER medication should treat the chronic pain experienced by a pt. The IR preparation is indicated for breakthrough pain. The IR dose should be calculated as 10-20% of the total OME dose a pt takes daily. Fentanyl patches should last 72 hours
Patient-Controlled Analgesia (PCA)¶
- Pumps can be programmed to deliver a continuous rate and/or a bolus dose
- Basal rate: a continuous infusion dosed per hour that cannot be adjusted by the pt
- Demand dose: a pt-directed bolus that is given at a prescribed frequency whenever the pt presses the button. Both the dose and frequency can be adjusted.
- The general rule of thumb is to calculate the total OME delivered through the demand when a pt is in steady state and convert 75% of this dose into the total continuous rate.
Calculating initial doses:¶
- Basal dose: Check what the pt is actually taking at home (may be different than what is prescribed, use OME). Take the total daily dose and convert to IV and then divide that by 24 hours to get an hourly rate. If moderate pain, increase dose by 25-50%; if severe, by 50-100%.
- Demand doses: The bolus dose should be 10-20% of total daily dose. The availability is based on the half-life of the medication (2hr for IV). Adjust the availability based on how frequently you want pt to be able to have a demand dose (e.g. if q10min divide by 12 or if q15min divide by 8 for 2 hours)
- Don’t forget to set lock-outs (maximum dose that can be given over a certain period of time) that includes both basal and demand doses
- Remember that the basal rate will not get to steady state for at least 8 hrs. When you admit pts or are transitioning to a PCA, always initiate the PCA pump with a bolus (or loading) dose How to Order PCA at VUMC
- Select Analgesic:
- *Hydromorphone (most common): Order “Hydromorphone (DILAUDID) PCA”
- Fentanyl (if on at home; not a good inpt PCA): Order “Fentanyl PCA”
- *Morphine: Order “Morphine PCA”
- Select “[Analgesic] PCA syringe” and adjust the following to pt’s needs:
- PCA Dose (“Demand”): amount the pt gets when s/he presses the button
- Lockout Interval: time between which “demand” doses will not be administered if s/he presses the button (i.e., the PCA “locks out”)
- Continuous Dose (“Basal”): amount the pt gets per hr in continuous infusion
- Max Dose: maximum amount of analgesic (Basal + Demand) pt can get in 24 hours
- Select “IV Carrier Fluid Options”> Choose Fluid option
- Select all “PCA Nursing Orders”
How to Order PCA at VA:¶
- Under Orders, select “Pain/Sedation Infusions”
- Under “PCAs,” select Analgesic of choice (Hydromorphone or Morphine)
- Adjust the following:
- Load: amount the pt will receive on initial set up of PCA
- Basal: amount the pt gets per hour in continuous infusion
- Demand: amount the pt gets when s/he presses the button
Interrogating PCA (to determine amount of analgesia pt received):¶
- Look at IV pump display and hit “Channel Select” on PCA
- Select “Options” in bottom left of IV pump
- Select “Pt History” on the left of the screen. This shows the administration history for a certain time period (e.g., 24h, 12h, 4h, etc.)
- Hit “Zoom” on bottom of screen to change time period to 24 hours. Should show:
- Total Drug: total amount of drug received in last 24 hours
- Total Demands: amount of times the pt had pushed the button for demand dose
- Delivered: amount of times the pt actually received a demand dose
- The difference between “Total Demands” and “Delivered” is the number of times the pt pushed the button without receiving a dose
- If you have questions about interrogating the PCA, ask the nurses. They are a great resource.
Opioid Side Effects¶
- Constipation: Dose-dependent and will not develop tolerance. If pt is taking opioids, s/he need robust bowel regimen (MiraLAX, senna) with goal of BM ≥every 3 days
- For opioid-specific constipation can do SQ RelistorTM (methylnaltrexone), but this is expensive and can only be given in the PCU or oncology floors at VUMC. For pts with chronic opioid-induced constipation as an outpt, can trial oral agents like MovantikTM (naloxegol). Can also consider PO naloxone but it does have small amount of bioavailability so watch for systemic reversal.
- Nausea: Occurs with opiate naïve p. Consider starting an anti-emetic concurrently. Most pts will develop tachyphylaxis with this over a day, so the antiemetic can be discontinued
- Urinary retention: Consider role of opioids in pts with new-onset or worsening urinary retention. Try to de-escalate opioid dosing if possible.
- Overdose: In pts with apneic emergency, IV 0.4 mg Naloxone; however, low threshold for multiple doses until response. For pts prescribed opioids as outpt, need naloxone 4 mg intranasal.
- If a pt with chronic opiate dependence is over sedated but not in immediate danger of respiratory failure, one can 1) hold the dose of opioid and let them wake up on their own or 2) give a dose of naloxone 0.02-0.04mg (1/10 of the usual dose). This latter strategy prevents opioid withdrawal and precipitation of pain crisis in pts on chronic opioids
- Pruritis: Due to histamine release from mast cells; can be treated with antihistamines. The opioid can also be rotated. Some but not all pts will develop tachyphylaxis.
- Toxicity: Hyperalgesia and neuroexcitatory effects (AMS, myoclonic jerking, seizures). Risk factors for neuroexcitatory effects are rapid titration, dehydration, and/or renal failure. Treatment is to rotate to a higher potency opioid and hydrate when possible.
Non-pharmacologic Therapies¶
- Procedural Intervention: best utilized when there is a specific, targetable
- Referral to chronic/interventional pain management (Nerve blocks or Radio-ablative therapy)
- Adjunct therapies: Pt’s will have varying opinions and responses on adjunctive therapies, but these can be as important as any pharmacologic therapy. CBT, personalized exercise regimen, PT/OT, chiropractor, acupuncture
- Additional Resources for Residents
- Pain Management Center at VUMC
- Pain Clinic at the VA. Would specify whether or not you are OK with them initiating opioids.
- Complementary and Integrative Health consult at VA
- Osher Center for Integrative Health at Vanderbilt