Prognosis¶
Liana Mosley
Background¶
- Prognosis is estimating the likelihood of an outcome (morbidity, mortality) due to a medical condition and can help guide clinicians, pts, and families in medical decision making.
- Pts frequently cite life choices rather than medical decisions for wanting to know prognosis.
Estimating prognosis¶
- Tools
- Should be specific to each pt’s situation (type of cancer, transplant eligibility, co-morbidities, etc.)
- Non-disease specific tool: https://eprognosis.ucsf.edu/
- Errors
- Studies suggest that clinicians consistently overestimate survival
- Two factors most associated with clinician error
- More clinical experience correlates with less prognostic error
- Longer duration of pt-clinician relationship correlates with more prognostic error
When to discuss prognosis¶
- Several studies suggest that across age and cultural background, most pts want their physicians to discuss prognostic information with them
- Ideally clinicians should discuss when the pt is not acutely decompensating and can process information
- Earlier prognostic discussions have been shown to decrease rates of hospitalization and highly aggressive care (chemotherapy, pressors) in terminally ill cancer pts
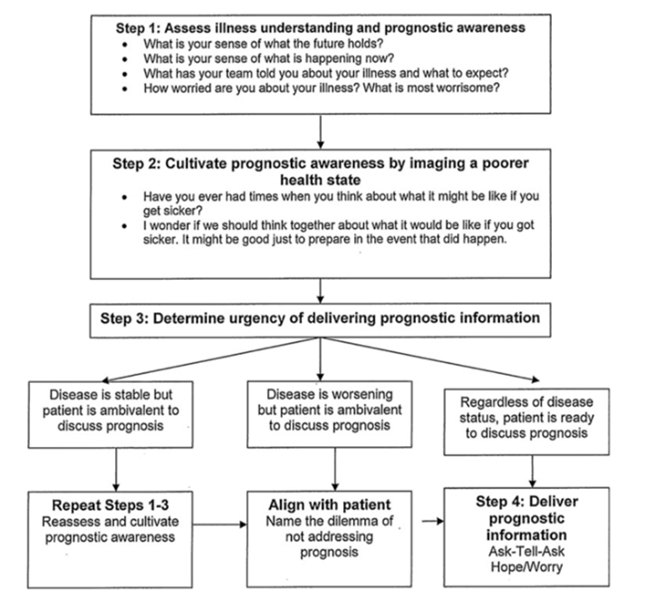
How to discuss prognosis¶
- Common Four-Step approach
- Confirm that the pt/family are ready to hear prognostic information
- Present information using a range: a few days to weeks; 2-4 months
- Allow silence after you provide information; respond to emotion
- Use prognostic information for eliciting end-of-life goals
- Ask-tell-ask
- Ask the pt what type of information would be most useful for them
- Provide information
- Ask pt if that answers their question or if they have additional ones
- Pairing hope and worry:
- “While I hope that x might happen, I worry that y is a possibility.”
Other:¶
- Helpful phrasing for pts and families resistant to discussing prognosis
- “In order to make this decision, it would be helpful if we talked about how much time you might have left to live. What are your thoughts on discussing this information?”
- “If you knew time was short for you, what would be important to you in making this decision?”
- The Palliative Care Network of Wisconsin has several helpful “Fast Facts” on determining/ communicating prognosis for specific disease states:
- https://www.mypcnow.org/fast-fact/prognosis-after-stroke/
- https://www.mypcnow.org/fast-fact/prognosis-of-anoxic-ischemic-encephalopathy/
- https://www.mypcnow.org/fast-fact/prognosis-in-hiv-and-aids/
- https://www.mypcnow.org/fast-fact/prognosis-in-decompensated-liver-failure/
- https://www.mypcnow.org/fast-fact/prognosis-in-end-stage-copd/
- https://www.mypcnow.org/fast-fact/determining-prognosis-in-advanced-cancer/