Delirium¶
Ben Johnson, reviewed by Jonathan Smith and Daniel Daunis
Background¶
-
Definition: acute (hours to days) fluctuating disturbance of attention and awareness due to an underlying medical condition
-
Complex and multifactorial condition, often due to underlying condition, with unknown pathophysiological mechanisms
-
Increased morbidity, mortality, and functional decline
-
Presentation: deficits in attention, orientation, or memory; hallucinations or delusions; sleep-wake disturbances; psychomotor changes (hyperactive, hypoactive, or mixed); language impairment; anxious or depressed mood, and/or emotional lability (agitation)
-
Think about the ABC’s of Delirium
-
Affect (anxiety, paranoia, irritability, apathy, mood shifts, personality changes)
-
Behavior (hallucinations, restlessness or agitation, psychomotor abnormalities, sleep disturbances)
-
Cognition (impaired memory, disorientation, disturbances in speech)
-
-
-
Delirium can persist despite identification and reversal of underlying causes, particularly in older patients or those with baseline cognitive deficits.
Evaluation¶
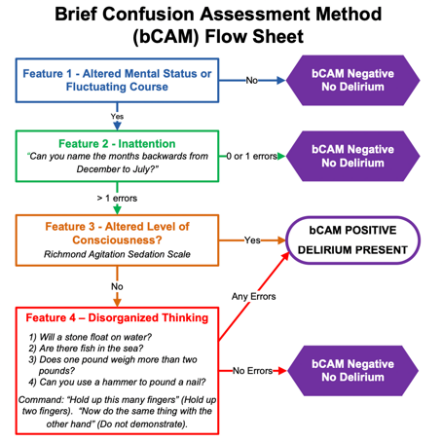
- Use screening tools to assess for delirium: Brief Confusion Assessment Method (bCAM). See critical care section for the ICU version, CAM-ICU
-
Once delirium is diagnosed, evaluate for the underlying cause. Delirium has many etiologies and may occur alone or in combination (in ~10% of cases, no clear cause is found)
-
Mnemonic for common causes of delirium:
-
D- Drugs/toxins (use of benzodiazepines, opiates, anticholinergics, steroids, etc., withdrawal from ETOH, benzos, etc.)
-
E- Eyes/ears (sensory deficits)
-
L- Low perfusion states (MI, PE, heart failure, sepsis)
-
I- Infection
-
R- Retention (urine, stool)
-
I- Intracranial events (trauma, seizure, stroke, hemorrhage)
-
U- Undernutrition/dehydration
-
M- Metabolic, endocrine (Hypo or hyper Na, hyperCa, uremia, thyroid, hypoglycemia)
-
-
-
Workup
-
History
-
Review current medications including those recently started or discontinued, as well as drug interactions
-
Review alcohol, sedative, substance use
-
Assess for pain and discomfort
-
-
Vital signs
- Temperature, O2 sat, POC glucose, and orthostatic vitals
-
Physical exam
- Assess for infection (SSTI, UTI, pneumonia, meningitis), abdominal pain, and sensory impairments, FND
-
Labs
-
CMP
-
Renal and hepatic function for changes in metabolism/elimination of medications
-
Glucose
-
-
Ammonia
-
Serum medication levels
-
Magnesium
-
TSH and free thyroxine
-
Infection – U/A, CXR, blood, urine, and sputum cultures
-
CBC
-
B12, folate, vit D
-
-
Imaging
-
CTH – non-contrast unless unable to get MRI (stroke, large structural changes)
-
MRIb with contrast (stroke, infection, inflammation, more subtle structural changes)
-
-
Medications - review anticholinergics, sedatives, opioids
-
Are changes needed to address pain control, constipation, insomnia, nausea, etc?
-
Substance use – evaluate for EtOH or BZD withdrawal state
- Empirically load on thiamine (500mg IV tid x9 doses)
-
-
EEG – evaluate for seizures, confirm presence of encephalopathic changes
-
LP – if concerned for CNS infection, inflammatory condition
-
Management¶
-
Treat underlying cause as above
-
Cognitive impairment or dieorientation
- Provide clock, calendar, and appropriate lighting
-
Regular reorientation
- Provide cues from a familiar environment (pictures, calls or visits from family members)
-
Ensure hearing aids, glasses, and dentures are available
-
Maintain normal sleep-wake cycle
- Keep lights on in the day and avoid excessive naps
-
Early PT, OT interventions, mobilization, move to bedside chair when able
-
Remove medical support devices as able (foley catheters, restraints, telemetry)
-
Ensure adequate bowel regimen and hydration
-
Assess for pain and treat appropriately
-
Medication reconciliation to reduce or eliminate total anticholinergic load, and to reduce or eliminate other deliriogenic medications as able
- See Beers criteria
-
See critical care section for prevention in the ICU (ABCDEF bundle)
-
Note on pharmacologic management: There is no pharmacologic intervention known to prevent or treat delirium. Medications for agitation only treat certain behavioral symptoms of delirium, are typically ineffective/harmful for hypoactive delirium, and do not modify the underlying pathological process. Reserve medications for agitation impairing patient safety when non-pharmacologic interventions alone are unsuccessful. See agitation section for medication approach